What is a middle ear infection?
What is a middle ear infection?
Middle ear infection, also known as otitis media, refers to infections that occur in the middle ear space, which is located between the eardrum and the inner ear and is surrounded by air-filled bone cavities. These infections are typically caused by viruses or bacteria and can be related to recent colds, the flu, or allergic issues. In most cases, both ears are affected.
How does a middle ear infection develop?
Middle ear infections are generally caused by bacteria or viruses. In children, these agents can easily travel from the throat to the middle ear through the short Eustachian tube. The microbes that reach the middle ear settle there and multiply. This condition affects the Eustachian tube, which is closely related to the middle ear, causing the mucous membrane lining the tube to swell. Due to the blocked tube, pressure drops, and the eardrum is pulled inward. The loss of flexibility in the eardrum results in reduced sound transmission. On the other hand, the fluid produced by the established microbes inside accumulates in the middle ear, pushing the eardrum outward, and causing it to bulge.
What are the factors that make middle ear infections more likely?
Middle ear infections are more common in children, especially those under the age of five, because their middle ear anatomy is not fully developed. Compared to adults, children have shorter and more horizontal Eustachian tubes, making it easier for germs to reach the middle ear during upper respiratory tract infections.
Factors that lead to nasal congestion can increase the risk of middle ear infections. Conditions such as adenoid hypertrophy, allergic rhinitis, acute and chronic sinusitis, nasal polyps, frequent bouts of the flu, and colds can contribute to middle ear infections. Immune system deficiencies, dysfunction in the muscles responsible for opening the Eustachian tube (tensor veli palatini and levator palatini muscles), and congenital anomalies (cleft palate) can also lead to poor aeration of the middle ear. Tumours in the nasopharynx region can block airflow to the middle ear, creating a conducive environment for infection.
How are middle ear infections classified?
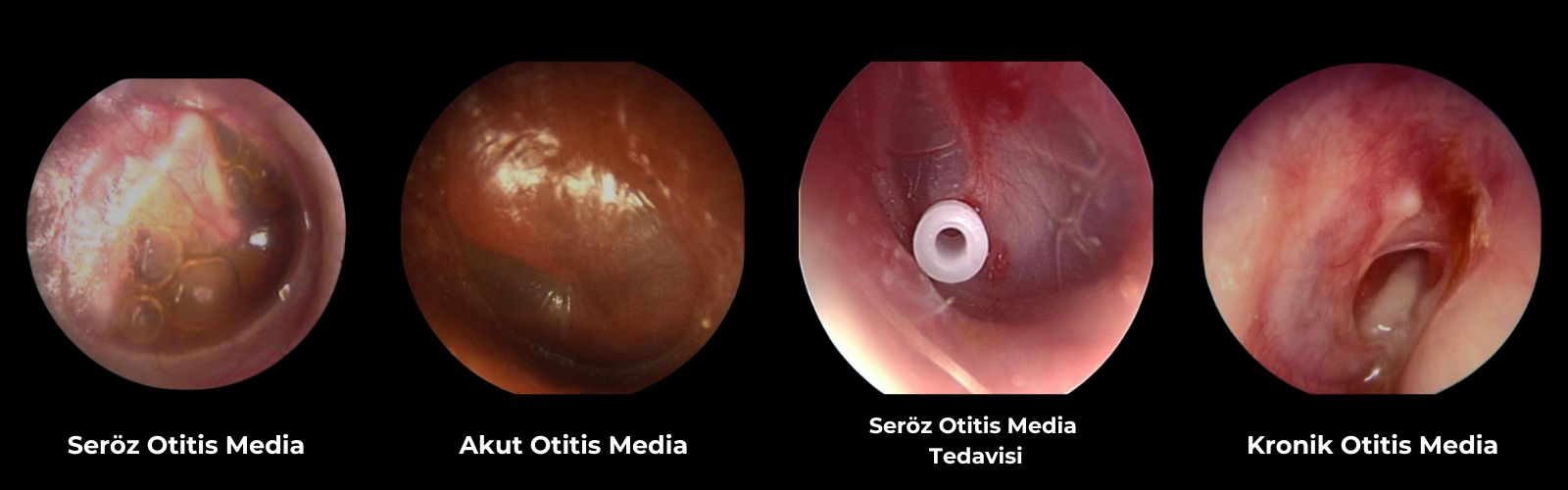
Middle ear infections are classified into four groups based on their duration:
- Acute Otitis Media (Sudden Onset): Middle ear infections that last up to three weeks fall into this category. The disease typically resolves within three weeks.
- Subacute Otitis Media (Unresolved Middle Ear Infection): Middle ear infections that last for more than three weeks but less than three months are considered subacute otitis media. Middle ear effusion (accumulation of fluid in the middle ear) that occurs after acute otitis media and resolves within three months falls into this category.
- Chronic Otitis Media (Prolonged Middle Ear Infection): These are middle ear infections that persist for more than three months. They are characterized by a perforation in the eardrum and discharge from the external ear canal. They present with conductive hearing loss. If drainage continues for six weeks after an acute suppurative middle ear infection, it is classified as chronic otitis media. The three-month duration is not strictly followed for these types.
- Chronic (Prolonged) Effusion-Related (Fluid) Middle Ear Infection: This category includes middle ear infections that occur following an acute middle ear attack and involve fluid accumulation in the middle ear that persists for more than three months.
At what ages is it more commonly seen?
Middle ear infections are more common in the pediatric age group. Considering that approximately 85% of all children experience at least one episode of acute otitis media, the importance of the disease becomes evident. Several factors contribute to a higher prevalence of acute otitis media in children. Until the immune system matures fully, especially in settings such as daycare, nursery school, and primary school, children frequently encounter upper respiratory tract infections. The shorter and more horizontal course of the Eustachian tube in children compared to adults allows upper respiratory tract infections to easily reach the middle ear. In addition to this fundamental mechanism, factors such as feeding while lying down (milk can easily reach the middle ear in children who drink from a bottle while lying down, potentially leading to infection), food allergies, passive smoking (especially continuous exposure of babies and children to cigarette smoke), and chronic adenoid tissue (adenoids) infections are risk factors.
What are the symptoms?
In middle ear infections, symptoms may include ear pain, ear discharge, hearing loss, ear itching (especially in young children), bringing the hand to the ear, as well as systemic symptoms such as fever, nausea, vomiting, loss of appetite, irritability, and diarrhoea.
What other conditions can it be confused with, and how can it be distinguished?
In infants, middle ear disease can be confused with various other illnesses because infants cannot express themselves clearly, and symptoms such as fever, restlessness, and vomiting can be associated with a wide range of diseases. Therefore, obtaining a thorough medical history from the family and conducting a comprehensive ear, nose, and throat examination are crucial for diagnosing the disease.
In adults, it can be confused with causes of ear pain. External ear canal infections are characterized by severe ear pain that worsens with movement of the ear canal. In particular, unilateral tonsil infections can cause ear pain on the same side. Pharyngeal (throat) tumours can cause referred ear pain. Infections related to teeth and impacted wisdom teeth can also cause ear pain. Temporomandibular joint (jaw joint) diseases can cause ear pain on the same side.
How is the diagnosis made?
In children, a detailed medical history and an ear, nose, and throat examination are typically sufficient for diagnosis. In general, the diagnosis of ear diseases is made through ear examinations under a microscope. Hearing tests (audiometry), tympanometry (measurement of middle ear pressure), temporal bone computed tomography, and magnetic resonance imaging of the brain are requested in some cases, especially those with complications (spread of infection into the intracranial space). These tests are crucial for diagnosis and treatment planning.
How is drug treatment performed?
In middle ear infections, broad-spectrum antibiotics that can pass into the middle ear are used. These antibiotics can be administered in the form of tablets or injections, especially in severe cases. Nasal decongestant sprays and tablets, along with mucolytic expectorants (to facilitate the removal of accumulated fluid in the middle ear), are given to help drain the fluid from the middle ear and reduce ear pain. If the patient's ear is discharging, they should be advised not to let water enter the ear.
When is the procedure to perforate the eardrum (paracentesis) performed in acute infections?
Paracentesis (perforation of the eardrum) has significantly decreased in recent times due to the availability of powerful antibiotics that can penetrate middle ear effusions (accumulated fluid). In very rare cases, when ear pain is severe and does not subside with pain relievers, and when the eardrum remains taut despite medical treatment, paracentesis may be performed to alleviate pain and reduce the tension of the eardrum.
What complications can untreated middle ear infections lead to?
If middle ear infections are not treated during the acute phase, they can become chronic. In this case, there may be ongoing ear discharge along with hearing loss. Modern medical treatments and surgical techniques have significantly reduced the incidence of chronic middle ear infections compared to the past.